I went through a laparoscopy to deal with hydrosalpinges and uterine adhesions, 26 months following the vaginal, non medicalised birth of my son, as well as two curettages and an abdominal surgery to fix the ensuing post-birth complications.
One of my tubes was completely compromised, the second one partially compromised and the uterus half covered by adhesions. I was told this was likely a consequence of the (many and invasive) post-birth interventions I had undergone.
The procedure was scheduled for 9 a.m. on the Friday before Christmas 2020. I was invited for the pre-op consultation days before, with a nurse and an anesthetist. More blood tests and an EKG. I was told to shower the night before and again the morning of the intervention, washing thoroughly my body, gradually advancing top to bottom, with iso-betadine received. I was to avoid any fragrance, perfume, cream, as well as shaving the few days prior.
I went in at 7 a.m. Little gosling was still sleeping. My husband kissed me goodbye and I took the metro to the hospital. It was still very dark outside and the air was crisp. It felt kind of lonely, but we had no one to ask to babysit. Mr Obama was reading to me from his book in my headphones. I carried a backpack with me (completely pointless, as it would turn out, but I was following the hospital’s recommendations) – phone, charger, Ipad, headphones, a book, a pj, slippers, a towel and a change of underpants. I was, apparently, geared up for boredom :))) during my scheduled one night stay in hospital.
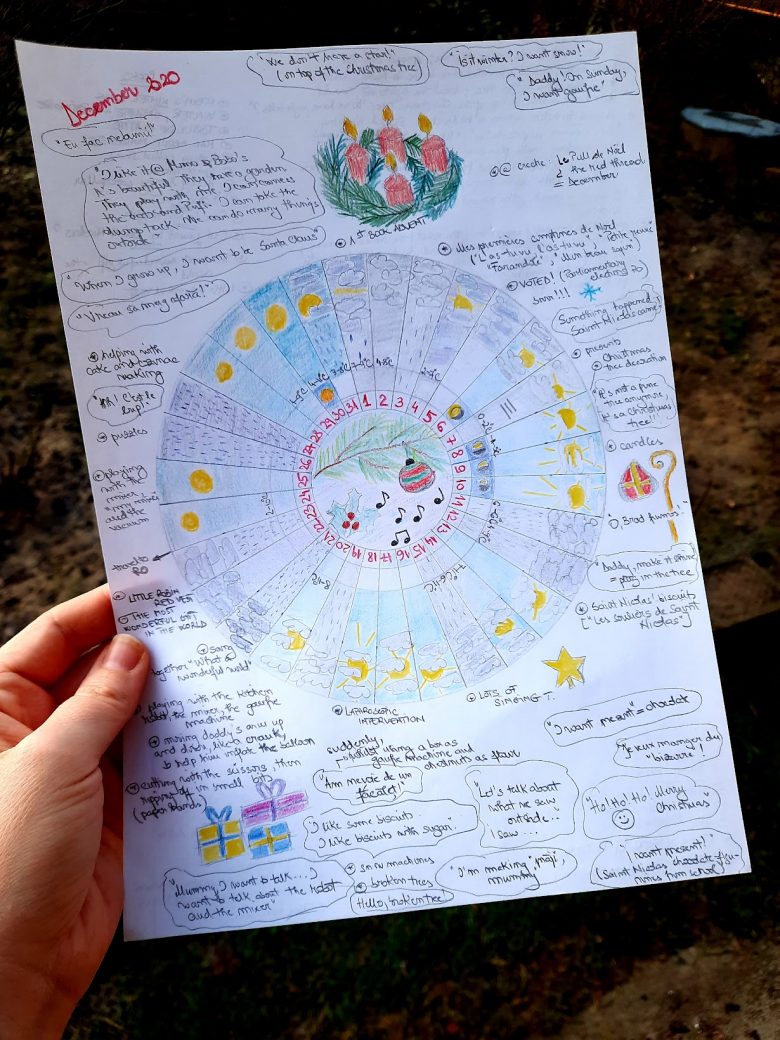
We had explained to little gosling (2yrs 8 months at the time) that mummy would be away, in hospital, undergoing an intervention whilst asleep for a day and a half. It was the first night we spent apart since his birth. No visits were allowed (COVID safety regulations), but we could talk over the phone. Daddy would be taking him to and fro the nursery, read to him the next book from our book Advent calendar and he could sleep the entire night in mummy and daddy’s bed. He seemed to understand, although he did ask for mummy and for tzatzi a couple of times during the evening/night.
After a quick registration procedure, I got a white plastic wristband, complete with a barcode (which was scanned every time I was moved and changed rooms) and my photo on it. I proceeded on my own to the extremely quiet maternity ward. I checked into my private room (the only way to guarantee that the intervention would be assigned to my obstetrician of choice) and changed into the hospital gown and panties I was given. A training nurse came in to shave my lower abdomen (at pre-op I was advised to avoid any shaving/hair removal the preceding days) and helped me put on compression socks. I drank the Xanax she left for me with just a small sip of water. I was feeling thirsty and hungry by now. I lied down. I read a bit, but mostly dozed off, waiting to be taken to theatre. I felt quite emotional, with tears coming to my eyes. I put on the new mask given by the hospital, just in case. I watched the short video my husband had sent with my son, delaying getting dressed for school, singing and saying hello to me into the camera. So sweet!
The scheduled time passed without anything happening. At 9.45, a stretch-bearer took me down, scanned my wristband and “parked” me in the big waiting room of the operatory block. It was a big hall, with mobile beds parked perpendicularly to the wall, separated by curtains. Nurses, doctors and “bed couriers” were coming in and out. More patients came and went almost immediately, their beds pushed by their operating nurses or anesthetists. I stayed put. I kept quiet and still, listening to the chatter next to the other beds. I was drowsy and had no sense of the passage of time. I asked the nurse in charge of the waiting room for the time – 11.15h. Hmmm… No idea when all that time had slipped by. It took a while longer before the anesthetist came, apologised for bringing me down too early and pushed me towards the theater. I climbed onto a higher mobile bed, my wristband was scanned again and off we went.
In the very well lit theater, the table stopped under a huge light. A nurse put electrodes to monitor the heart rate on my chest and somewhere on the back, the blood pressure thingy, then wrapped my right arm safely alongside my body. The anesthetist installed the drip, whilst telling me a joke from one of Louis de Funes’ movies. I was covered with an extra green blanket – I was cold and shivering. My hand started to hurt when the drip started flowing. The doctor slowed down the flow. He held a mask on my face; my hand started to hurt all the way to my elbow and I lost consciousness before I could finish telling him that.
Next thing I know is waking up with pain in the lower abdomen, much like strong menstrual cramps. I was feeling heavy. Had this constant need to clear my throat to be able to speak. I was feeling groggy. A nurse was busily moving around my bed, hanging things. I could feel pressuring and letting go of my arm, followed by a beeep, the thingy measuring my blood pressure. I was in a haze for most of the time I was conscious in the recovery room. The nurse kept talking to me. She gave me painkillers and placed a hot water bag on my tummy to ease the pain. At some point, I located a clock on the wall in front of me – 14.15h. I tried to calculate how long I had been under, but found it impossible to be precise. At 11.15 I was still in the waiting room, but my sense of time had already been altered by then. And who knew how long it had taken me to open my eyes after the procedure?
I thought to check the bandages, to make sure things hadn’t gotten wrong and there was no big cut. I slowly took my hand under the blanket and felt small pieces of bandage here and there on my abdomen. Oh, good! I felt relieved. It had stayed laparoscopic…
I could feel the hotness of the water bag and kept moving it around my tummy. At one point, my bed was moved to one side, waiting for a stretch-bearer to take me to my room. A different person, chattier, took me back up. He made small talk, but I can’t remember what it was about. It felt like my stay in the recovery room had been very short, but by the time I was back in my room it was past 16.00h. I sent a quick message to my husband.
My throat cleared out quickly. I still felt the menstrual-like cramps and some stingy sensations alternating between the cuts, one at a time. I pulled up my shirt and counted 5 small squared bandages: 1 in the navel, 3 in the lower abdomen (middle, left and right a bit higher), one above the navel on the left side. I was intrigued: why so many? Why the one above the navel? I suddenly felt hot and I took away the additional blanket they had put on me in the theatre.
A nagging sensation to pee came to me. A nurse helped me get up slowly from the bed and then waited outside the bathroom door. I pulled up the hospital shirt and looking down, there was suddenly more blood than I had anticipated and it started flowing down my legs, staining the compression socks.. I asked for help, I was too slow… I sat down, but did not manage to pee in the end. The nurse called for help and they helped me back to bed. I felt dizzy and a bit nauseated. “Call us when you want to get up again”, they told me.
The nurse came in regularly to check my temperature, blood pressure, the bandages for any further bleeding, as well as for any vaginal bleeding. All normal. She warmed up my water bag as well. That helped a lot.
I called my husband and parents. They had been worried. I had gone into surgery three hours later than scheduled, so my husband had immediately feared complications. He had called the ward to ask after me. I could sense my parents were also relieved. I wrote back to my best friends who had left messages of encouragement during the day.
At some point, the pain came back. The perfusion got stuck and the nurse could not manage to fix it. She called the anaesthetist to ask whether she could change the whole thing, but couldn’t reach him. He had just passed by my ward minutes earlier and was possibly on his way home. The surgeon told her she could it take off completely and give me pills instead. Dafalgan forte every three hours or so. I also got a pill, good tasting, to put under my tongue and suck it. And, at some point in the evening, the much dreaded anti-clout injection in the belly came upon me.
The surgeon stopped by to see me in the evening. He gave me a quick summary. He had taken out the right tube. He had saved the left tube, but “it wasn’t exactly beautiful”. He had cleared the adhesions in the uterus and he had spread a gel all over to prevent further adhesions from forming. Half of the uterus was closed; “all sorts of things had happened inside” he said. He told me to drink a lot, stay hyperhydrated. Gave me the medical leave paper and prescribed me antibiotics for the next five days.
Afterwards, I dozed off, woken up only by the nurse’s visits. The night nurse told me to drink water and call for help to go to the toilet. I had to pee before midnight. I drank 1l and a half of water and waited… two hours until I felt any need to pee, not remotely as pressing as I would have thought after drinking that amount of water in one hour! Victory!!!
Around the same time, my shoulder started to hurt, around the clavicula. Sharp. Numbing. It came and went. It felt particularly poignant when I stood up and went to the toilet. No more dizziness, but it came with nausea. Keeping it warmly tucked under the blanket helped. I rubbed it with my other arm and put my head on it, kind of like hugging it. Pain in the abdomen was now localized between the five cuts, not anymore focused on the lower abdomen. It was surprising to me to learn this was absolutely common after a laparoscopy, an effect of the CO2 they put inside the abdomen to dilate it during the intervention. It takes a while to make its way out of the system.
I went to sleep listening to Mr Obama. Between midnight and 6.00 all was quiet. I woke up a couple of times, either to go pee or to adjust my position. My feet hurt, swollen in the compression socks.
Early morning, after the usual checks (everything was in order, very little vaginal bleeding, bandages same as the previous day, no fever and my usual low blood pressure), I peed again. It seemed like “the” milestone to meet, my nurse was very interested in it. My bandages were changed. I decided it was time to go for an extended walk around the ward. I felt bloated. My shoulder pain kept coming and going, particularly when I stood up. It went all the way from the stomach, with some nausea, through the diaphragm, all the way up into the right clavicula and then through my right arm all the way down to the pinky finger. I had read that walking should help.
The anesthetist came again and prescribed me a diclofenac for my shoulder pain. A kinesitherapist subsequently came by to check on my shoulder. All was within parameters.
I left the hospital on my feet right after lunch. My husband and little gosling were waiting for me outside. The little one had fallen asleep in the car seat. My backpack felt heavy. I realised I could have gone with just my phone and headset to the hospital. Anyway, better to be prepared for the worst.
The laparoscopy was a success. The best result possible had been achieved, no miracles. Out of the hospital, I felt no more pain in my abdomen. However, the pain in my right shoulder was strong and numbing. The worst was between 18 – 36h post-op. During the same period, gases were also quite painful, particularly so when lying down. The second night after the intervention was difficult. Without the adjustable hospital bed, my improvised pillowed backrest was much less comfortable. It was also a struggle to keep little gosling at distance from my tummy. It took a lot of explaining as to why we needed to be more careful for a while.
Later on, together in the bathtub, with the bandages off and the cuts still visible, little gosling would ask what happened. I told and retold him how those many tiny cuts on my tummy had come about on the occasion of our first and only night apart, so far.
Four days and a half after the laparoscopy, we flew home for Christmas. A two hours and a half flight. I was anxious, as I had read that gases in the intestines dilated at least 30% at great heights, and was afraid of pain and discomfort. The surgeon had reluctantly given me a green light to fly; he would have preferred I waited, but it was already the 23rd of December. The International Civil Aviation Authority indicated on its website it was safe to fly 2 days after a laparoscopy. So, we took a chance. All went well, no sensations whatsoever. I spent two weeks convalescing at my parents’ home, reading books and doing little of anything else, whilst little gosling was enjoying his grandparents and their garden and animals, in the mild winter weather.