The post Let’s Go to the Museum: first visits to the “car museum” appeared first on Mommy Goose Chronicles.
]]>As far as museums go, little gosling has taken to visiting repeatedly the ones concentrating on things that move: trains, trams, cars, planes. Whilst we’re yet to visit the tram museum (only open in the afternoons), we’ve seen the others at least twice each over the past months. Great opportunities for quality time together in an instructive, exciting, playful setting and for little ones to use energy. This is particularly true for us when wether makes us less inclined to spend time outdoors during the weekends.
The car museum (“Autoworld”) is accommodated in a big hall with plenty of space. This allows little gosling to run around, which is what he mostly does, on fast forward  without much chance of knocking down fragile exhibits. It displays a varied collection of over 250 European and American automobiles from the late 19th century to the 1990s. It is notable for its collections of early and Belgian-produced vehicles and several limousines belonging to the Belgian royal family. Interestingly, there are corners displaying horse drawn carriages, as well as mechanical workshops and different engines.
without much chance of knocking down fragile exhibits. It displays a varied collection of over 250 European and American automobiles from the late 19th century to the 1990s. It is notable for its collections of early and Belgian-produced vehicles and several limousines belonging to the Belgian royal family. Interestingly, there are corners displaying horse drawn carriages, as well as mechanical workshops and different engines.
There’s also a corner dedicated to the French comics’ character, Michel Vaillant, featuring an F1 real size car maquette. This was obviously the highlight of our first visit. What can be better than getting into a car and pretending to drive? If one does not take into account climbing on to the wheels or trying to make them turn. Of course, there was time for drawing, snacking and reading a story.
First time around we looked at sizes of cars, wheels, steering wheels, comparing them. Most of all, we played at identifying their colours. The second time we went, he went ahead and we followed. He would stop in front of a car, pointing and asking: “What is this car called? How fast can it go?” Brand of the car, year of fabrication and, most importantly, the maximum speed it could reach. We compared the size of cars and their lights and identified the convertible ones (“this can only go in summer, it has no roof”).
A temporary exhibition of racing cars attracted most of our attention. Little gosling loved the sound of the Italian brands . He was completely in awe with the big numbers I blurted out for the maximum speed they could reach.
We hardly ever cover the entire museum in one visit, which is ok. The aim is to stay as long as he is enjoying the experience, but not long enough for him to get tired. The ideal duration would be around an hour, but we can hardly stick to it. Little gosling gets overly excited about trips to the museum and insists on seeing everything.
Make time for snacks and reading
After the initial burst of energy and running around, it is pretty quickly that I hear “Do you have something to read? Do you have to eat?” We never leave home without snacks. I find it important we make some time half-way through the visit for a snack break. As a result, we avoid tiredness and hunger setting in and communication difficulties. We usually take along a combination of fruits (banana or bite sized strawberry or apples), nuts (cashew, pistacchio, peanuts), cubes of cheese and salami and bretzels or corn cakes. In less restrictive times, we take advantage of the museum cafeterias to enjoy a hot chocolate and a biscuit or a sandwich.
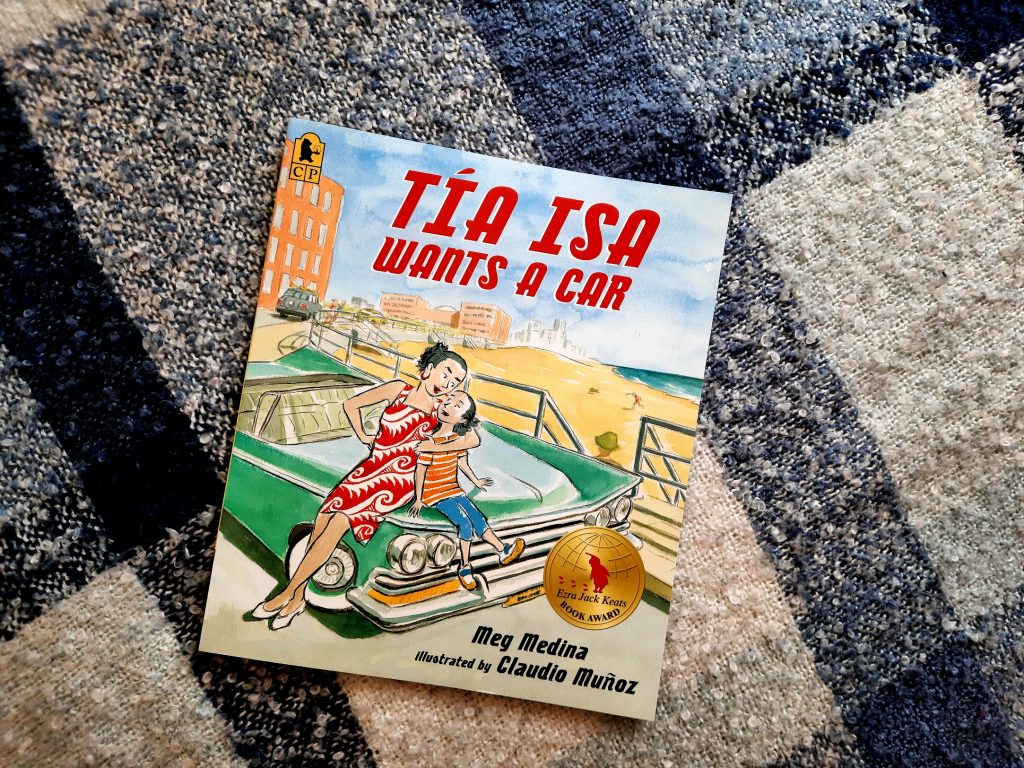
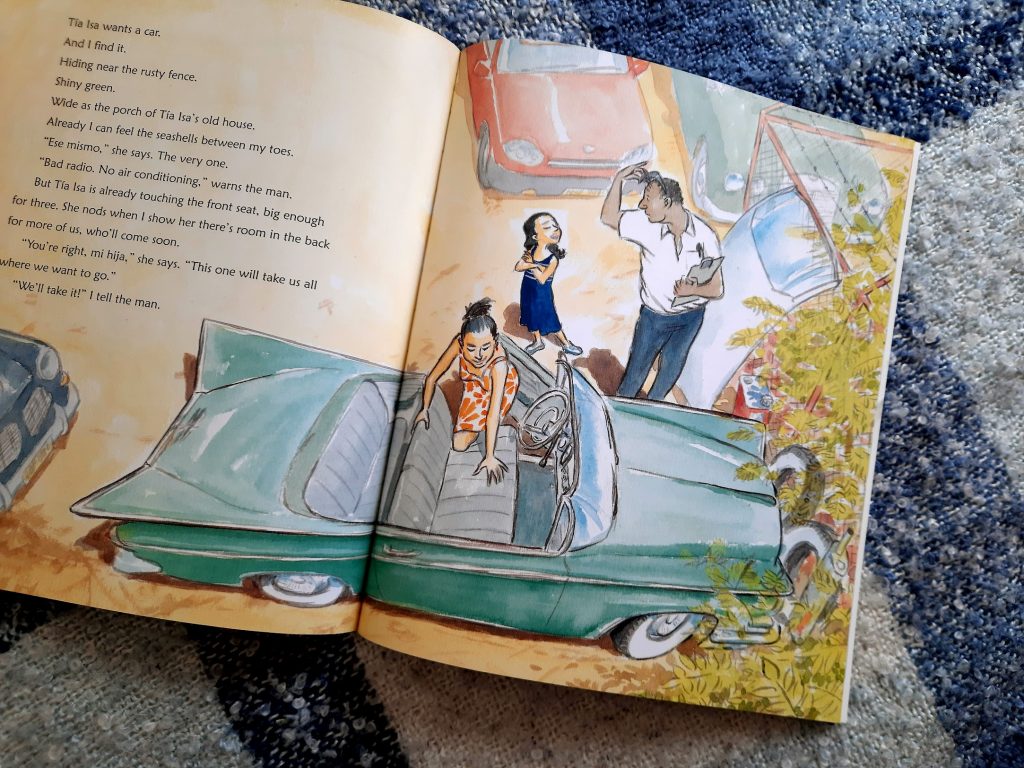
“Tia Isa wants a car”
Equally, I always carry picture books in my bag when we go out. We never know when we may feel like reading ;). The first time we read “Tia Isa wants a car”. This, as it turns out, is the our only story featuring a car.
I loved the story the first time I heard it read aloud by Meg Medina on Julie’s Library podcast. An immigrant family: aunt, niece, uncle, working to support their loved ones back at home, on the island. Reminiscing about their house by the beach and dreaming about the day, soon, when they will be all together again in their adoptive place. The aunt wants a car, green like the ocean, with wings like a swooping seagull, to take them all to the beach. Little gosling loved that idea: to get a car to take us to the beach! The niece secretly starts doing small chores in the neighbourhood, to put aside money to help her.
It’s a wonderful, heartwarming story about family, separation, longing, nostalgia, kindness, community, effort, the value of work, joy. A touching introduction into the life of immigrants. An emotional perspective of being far from the loved ones, whilst constantly having them present, in mind and hearts. I found it incredibly moving that first thing they did upon getting into the car was sticking a photo of the entire family.
We definitely need more stories featuring cars and/or driving. And someday soon, we’ll watch “Cars” together :P.
Little gosling loves to spend time in the driver’s seat of our car, “Zambilica” (in English, “small hyacinth”). He emphatically tries to turn the steering wheel and touches the commands, pretending he is driving. This is his ritual for a few minutes every time we come back from a car ride. When he grows up, he would like to drive us around, with daddy and I taking turns sitting in front, next to him.
The post Let’s Go to the Museum: first visits to the “car museum” appeared first on Mommy Goose Chronicles.
]]>The post My (Second) Pregnancy Diary: Second Trimester Combination of Energy and Anxiety appeared first on Mommy Goose Chronicles.
]]>Finding out the sex of the baby
15 weeks into the pregnancy we received the results of the noninvasive prenatal test (NIPT). Just what we were waiting for to spread the word about our new baby. Little gosling wasn’t aware of anything, as we had taken care of not talking about the pregnancy in his presence. We wanted to be able to break it to him with all details, including the sex of the baby.
At the last consultation before our three week holiday in Romania, the gynae reassured us upfront the NIPT results were good, no anomalies detected, but wouldn’t reveal the sex until after the routine ultrasound. “On va voir ensemble” (“Let’s see it together”), he said. Baby was not in a favourable position to see anything so, at the end, he simply said: “C’est une petite princesse”. A girl!!! I so badly wanted the baby to be a girl. My husband was unshaken; he had been certain all along it was a girl. “It’s what I ordered” he kept saying :))).
Breaking the news to our son
Little gosling had expressed the wish to have a younger sister. His best friends at school, Gaby and Emile, had younger sisters in the same school, Lucia and Freya. Apparently, the siblings were a constant presence in their conversations. One night, little gosling told me: “Let’s have a little sister”. I was pleasantly surprised and I could see his daddy suddenly raising his gaze and paying attention to us from his corner. I explained that if we had a baby we could not really choose; what if it were a little brother? “I would just ignore him”, he said very naturally. Didn’t know how to react to that :))). So, good thing it was a little girl.
I already had a short list of girl names. It took us less than a minute to discuss and decide on a name, before we picked up little gosling from school and gave him the news. I listed them and my husband only liked one of them. Our baby girl would be named “Iulia”.
At home, we told little gosling we needed to talk to him about something.
“Do you remember how you wanted a little sister?”
“Yes? Is it coming?”
“Yes, you’re gonna have a little sister. Daddy and I thought of naming her Iulia. What do you think?”
“I like the name Iulia. Where is she?”
“In mommy’s tummy.”
“Can I see it? When is she coming?”
“In January. She’s gonna still grow in mommy’s tummy. She’s about 10 cm big now (approximating the length with my fingers). When she’s ready, she’ll come out.”
He was looking at us with big eyes, full of surprise and excitement. He was curious. That day and ever since, he’s been asking recurring questions about when, how long before Iulia comes out and how, which way she would come out of mommy, how she got into mommy’s tummy.
I explained calmly and naturally.
“Daddy planted a seed in mommy’s tummy, just like he did with you.”
“She will grow inside mommy’s tummy until she is big enough and ready to come out, just like you did. We expect her to come out of mommy at the end of January next year (after holidays, after mommy’s birthday, after St Nicholas and Christmas).”
“ She will come out through my vagina” and showed him when we took baths together.
He asked whether we could name her Lucia or Freya. “We want her to have her own name and identity. There is already one Lucia and one Freya”. He was ok with that.
It felt good, unpretentious, natural, intimate, the way I wanted it to be.
He has kept asking to see my tummy (skin, not covered with clothes) and caress it, calling Iulia’s name. When he sees me caress my tummy, promptly asks whether she is moving and quickly puts his small hands on to feel her. There’s a clear sense of impatience and he would like Iulia to come out already, including her in our conversations.
Bodily sensations
Second trimester brought along new sensations compared to my first pregnancy.
Round ligament pain was completely unfamiliar to me. The sharp ache in the sides of my abdomen, particularly when doing a sudden movement, like getting up or twisting in any way. I quickly learned to move gently and slowly, lifting my body up bit by bit when lying down.
The hunger sensation eased, almost to a point where I would feel hungry in the morning when waking, but pretty satious in the afternoon/evening. Reflux and particularly a sour taste in my throat, occasional heartburn settled in early. For a few weeks, I felt discomfort after eating anything made with white flour, so no more pains au chocolat :P. Can’t stand to see or taste broccoli anymore and ethnic food stopped agreeing with me.
I continue battling constipation, going from one extreme to the other, finding it hard to fix from diet alone and exercise. The pressure on my rectum keeps the piles alive and much more than during my first pregnancy, I struggle with internal piles. The anal itchiness is my constant companion, but the internal piles start to sting more and more often.
Breast tenderness has been less of an issue than during the first trimester, although there have been times when even the touch of the bra was absolutely uncomfortable. Little gosling has kept on breastfeeding, unbothered by anything.
One thing I have not missed at all from my first pregnancy: swollen ankles. Because I had no issues. Must be courtesy of Brussels weather ;).
I am still not sure how the famous Braxton-Hicks contractions are supposed to feel like, but mid-way through the second trimester I definitely felt the same sensations as during the real contractions during my first labour: abdominal cramps, low back pain and urges to empty myself. Honestly, these helped ease constipation.
Energy levels, sleep, exercise
From week 12 onwards I felt super energetic, I wanted to do so much. Good-bye tiredness! I slept like a log again, no longer waking up during the night to pee. What a relief! My body sort of slowed down towards the end of the afternoon, but generally, I felt like I could do anything.
I kept taking my morning walks, determined to do my 10 000 steps daily as long as possible, if not until the very end. It was my me time, listening to audio books or podcasts, observing the nature around our park, talking photos just for my soul, capturing the little details: the shapes of leaves, the swans chasing the geese away on the lake with their big white wings in this menacing basket-like shape, the flowers, noticing the noisy parrots, following the growth of chestnuts, noticing the same people running at the same hour every day or practicing meditation on the grass, under the same tree…
I mapped the different pre-natal activities in my area, looking for those with physical presence and working hours schedules, as online things did not work for me and I did not want to eat into little gosling’s time with me. Due to the pandemic and holidays it was only from September onwards that courses finally became available.
I started going to pre-natal yoga classes once a week at my favourite studio. It was almost one year since I had last gone to a yoga class and let me tell you, it was hard. My heels were way up high from the ground again in downward facing dog. The warriors felt uncomfortable on my knees and shoulders and I was back to the easiest version of the tree pose. My balance was off. But it felt good for my body, for my back, for my joints and for my mind. It was just the right amount of time and effort for my body at that point. And the 15 minutes of winding down in a reclined shavasana at the end felt heavenly!
I went to pre-natal aquafit once a week, with a practicing midwife. I enjoyed that tremendously! Being in warm water, with other mommies to be, sharing about our pregnancies, fears, doubts. I kept thinking how great it would have been to be able to swim and spend more time in water pregnant. One day, I’ll definitely learn to swim properly!
Weight gain/pregnancy bump
Weight gain was less than during my first pregnancy – less than 3 kg. I had the same high bump, right under my chest, for the first many weeks. At some point mid-way, it took on a more normal, equal, round shape and descended further down. I could not locate the box with my maternity clothes from my first pregnancy, so I bought two pairs of maternity shorts, for the warm weather and two pairs of maternity leggings for the cooler times and kept on using my tops. At 28 weeks I still used my longer blouses; they fit just fine.
Baby moving
I started feeling Iulia move around 20 weeks in. The gentle, fluttering, almost imperceptible kicks from the first days became more frequent and vigorous towards the end of the trimester. The last 3-4 weeks I was surprised by how active she was, especially at night. I could sleep very well, but little gosling had a period of waking up indecently early so we were all on our feet before 5 a.m. And Iulia was kicking to the point my tummy was shaking :)))) Little gosling had been such a calm baby in my tummy, so I feel surprised every time I feel her. I uncover my tummy and watch with wonder, laughing and talking to her, as her moves make ripples on my skin.
She also becomes very active when I read to little gosling. We joke that she must like the sound of our voice, rejoicing in the certainty that when she comes out, she will recognise us, she will know mummy and her older brother.
Pre-natal checks
I continued seeing my gynae once a month, with routine urine and blood tests performed each time. Toxoplasmosis was much more of a concern here than in South Africa. I don’t remember doing these tests the first time around. And I was determined to monitor my thyroid closely. My TSH levels were good on the hormonal dosage I had pre-pregnancy, so I kept it up unchanged. Somewhere along the way, though, I ran out of pre-natal vitamins and completely forgot about them.
Wasn’t too crazy about the cervical exam the doctor performed each time before the ultrasound. He explained he was doing it to make sure the cervix was closed and there was no risk of infection spreading up towards the uterus. Upon reading up, I understood it was not a routine procedure done by all gynaes, but there were moms for whom it had prevented serious issues. I talked it through with my overly-protective husband and we decided that whilst uncomfortable, we would rather not take any chance.
The second trimester morphological ultrasound was incredibly technical and detailed. Happily, all was within parameters. I don’t remember having done a special ultrasound during my first pregnancy. Back then, it felt like all our monthly ultrasounds were incredibly detailed (much more so than the routine ones this time), so maybe there was no need and our doctor was specialised in this.
I had my gestational diabetes test at the end of week 27. I found it such a peculiar experience, that I will detail in a separate post.
Preparation for birth
Keen on having a natural, unmedicated birth like the first time around, I started researching alternatives for giving birth in Brussels. Home birth was not an option we were comfortable with, but a midwife unit in a maternity hospital definitely was top of my preferences. It became quickly obvious there was little choice. While the system here sees C-section as a last resort, the overwhelming majority of births take place in hospital, overseen by gynaes, in the old fashioned lying on your back position with feet up and in 75% of the cases, with an epidural.
There were two options available. Luckily, one was in the hospital where my gynae was practicing and I decided to explore first his openness to work with a midwife led process. I can’t shake off the complications that followed my first birthing experience and kept thinking if I had to undergo an intervention, I’d rather do it with my doctor. After all, he did a good job with my laparoscopy.
In parallel, I read books and articles about maximising chances for a gentle birth; started listening to my hypnobirthing affirmation and relaxation tracks and practicing the breathing techniques. I attended the birth preparation classes given at my hospital by a specialised kinesitherapist, focusing on breathing techniques and positions in labour and expulsion phase. I missed the one on perineal education, though. They were quite useful to understand what to expect from birthing in my hospital of choice.
We kept the conversation going with little gosling about the progression of the pregnancy, baby’s birth and how we would all need to adjust and cooperate to take care of her. Much like we took care of him. We read stories about the arrival of siblings. We talked about what she would eat; about the fact that babies’ only way of communicating with us is by crying; about the fact that in the beginning they can’t talk or walk and spend most of their time sleeping.
We decided it was a good idea to ask my mom to come and stay with us for a while. A one way ticket, my husband called it. We talked to my parents and made arrangements for her to arrive around 4 weeks before the due date, just in case.. In Belgium, mom and baby are kept in hospital at least three days post-partum and with the pandemic restrictions, it was not entirely sure kids would be allowed to visit. My husband’s main concern was to make sure little gosling was cared for while he was with me during birth and in hospital.
We also decided that the only thing we really needed to have ready for Iulia’s birth was a bigger family bed. We would co-sleep, but that did not mean we would change anything in little gosling’s routine. He falls asleep in his bed, in his bedroom, but sometime in the middle of the night, he moves to our bed, between us. A bed of 2m x 2m would do. Not your typical size in Belgium. So, we ordered a mattress from a German company and my husband undertook the task of expanding our bed frame to fit it (I can hear him cutting the wood as I am writing this :)).
We kept all little gosling’s baby clothes and items, including pram and car seat, so no need for creativity there. Wasn’t too keen on blue for him, just as I am not keen on pink for Iulia, so his clothes should give us a good breathing space.
Uncertainty about birth
Once the NIPT results came back positive, my anxiety levels dropped. I felt relieved and I could relax, although not completely. Being a 39 year old mom-to-be, I was alert to the different increased risks, so kept counting the weeks and marking the different milestones we were safe from.
Anxiety levels went up after our 25 weeks appointment, when I opened the conversation about birth with my gynae, with the intention to understand his views on cooperating for a midwife-led birth. He enquired after my expectations and calmly said that based on the little information he had about my post-partum complications the first time around, he would recommend a C-section.
That was a big blow to me. All my hopes, expectations and plans were shattered. I asked questions, wanting to know the risks. I understood his concerns revolved around the recurrence/avoidance of the post-partum haemorrhage (what was the cause? Inability of the uterus to contract?) and a possible uterine rupture (How big had the uterus perforation during the failed querretage been? How had it been sutured? Where exactly on the uterus was it? Had there been any infection?). I did not have a detailed answer. He suggested I get a medical report from my caregivers in South Africa and continue the conversation on that basis.
I felt disappointed. I came out of the consultation with tears in my eyes. This was the very opposite of what I wanted. I worried that I wouldn’t be able to get the details requested in time. Luckily, my midwives and doctor in South Africa quickly provided me with the medical reports and I even got the post-surgery nursery reports from one of the hospitals. My gynae is yet to examine them in detail, but it may be less dramatic than he had imagined. The conversation about birth however, is a pending one and it may yet be influenced by the evolution of the pregnancy during the next weeks.
Risk of preterm birth
Week 27 added on a new layer of anxiety and frustration.
27 weeks and two days in, I ended up in the emergency room. One very early morning, I woke up with abdominal cramps, low back ache and the urge to go to the toilet. Nothing happened the first time around, but half hour later and yet another thirty minutes later I emptied my bowels. On the soft side. When nausea and dizziness added to the mix, I became scared. I threw myself onto the bed and asked little gosling who was awake and gently caressing me, telling me “don’t worry, mummy, it’s gonna be ok” to call his dad from the other room. I wasn’t feeling well. My husband called the emergency room and we were advised to go straight to the maternity ward.
Half an hour later, I was vomiting on the hospital’s corridors, as my husband pushed me in a wheelchair, with little gosling holding my hand. I was immediately accommodated into a single room, with monitors on to check my baby’s heart rate and detect any uterine contractions. I could feel her kicking very actively. It was 7 a.m., her peak time. I knew she was fine, but started wondering about the contractions. More than anything, I just wanted to feel better.
By then, pain on the sides of my middle back was quite strong. My husband took little gosling for breakfast to the cafeteria, whilst I waited for the doctor. I peed into a cup and the midwife took a blood sample. No uterine contractions were detected and baby’s heart was just fine. I kept moving around, trying to find a comfortable position. I got nothing for the pain, even though I asked several times if there was anything that could be done. At some point, I fell asleep. Two hours later I woke up and the pain had subsided.
The gynae came in, with the blood results and part of the urine test. Nothing extraordinary. A little anaemia, which wasn’t unusual. All pointed to a gastro virus possibly combined with a urinary infection. Nothing worrying so far. She did an ultrasound, including the first transvaginal ultrasound since the very beginning of the pregnancy. All looked fine with the baby, but my cervix was shortened (27 mm, below the 30 mm normal lower range) and showed signs of opening.
This meant I was at risk of premature labour. She prescribed progesterone three times per day and recommended bed rest. Going to the toilet and taking the occasional shower was ok; if I felt really brave, I could take a 10 min light walk, but that was it. I needed to do all possible to keep Iulia inside at least until 34 weeks or 2,5 kg. Seven more weeks.
I could choose to stay in the hospital, but I wanted to go home with my family. I wanted to go back to my life. Not to mention the financial implications of an extended hospital stay. That was ok, as long as my family would allow me to sit still and calm. No sexual contact, no stimulation of any kind, including nipple stimulation or caressing my tummy. The doctor then mentioned a hospital stay further down the road to have corticosteroid shots to help mature the baby’s lungs. I was tired and it was all moving too fast for me to process or ask any questions. I was just listening…
When she mentioned no nipple stimulation I naively brought up the issue of breastfeeding. She was most obviously surprised. It took her 30 seconds or so to react. Was I still breastfeeding?! She had seen little goslings in the corridors.. At three years and a half.. Absolutely no, that needed to stop. Breastfeeding could bring about uterine contractions, which was to be absolutely avoided.
The doctor repeated all these to my husband, who took it all in very seriously. He would make sure that I rested and did not get upset by anything. And we went home. Worried. Scared. Frustrated. We needed some time to process all the information and the implications…
The post My (Second) Pregnancy Diary: Second Trimester Combination of Energy and Anxiety appeared first on Mommy Goose Chronicles.
]]>The post My (second) Pregnancy Diary: First Trimester Anxiety and Discomforts appeared first on Mommy Goose Chronicles.
]]>My second pregnancy has felt nothing like the first one. Nothing more so than the first trimester. Anxiety has been at very high levels since the very beginning and bodily sensations were all over the place, resembling more my first third trimester. The world upside down, and then some more.
All websites on pregnancy, what to expect and week-by-week progress, have these very long lists of possible pregnancy symptoms that one may experience. In my first pregnancy, the first trimester was hardly out of the ordinary, aside from some nausea around noon, for a couple of weeks, that I washed away with some Schweppes. This time around, I felt more like the women those websites seem to be addressing.
The very first weeks were incredibly uncomfortable. Itchiness and stinginess all around my intimate area, pelvic and anal were annoying, making me feel very irritable and edgy and probably contributed to an increased anxiety.
Vaginal thrush
I had experienced a very mild episode of vaginal thrush immediately after the birth of my son, but it had all subsided with one or two applications of balm. What I felt now was plainly unbearable. It was itchy to the point it gave me spasms and made me jump up and want to scratch the hell out of it. This happened immediately after implantation, so very early on in pregnancy. My GP prescribed a vaginal cream and it took around a week to completely go away. It came back once more just before the end of the first trimester, but quickly subsided with cream.
Piles/haemorrhoids
I call them “my friends”. During the third trimester of my first pregnancy, I got myself three “friends”: two rather big ones and a tiny one. All external piles gathered together around my anus. Never painful or stinging, only itchy during pregnancy. They generally kept the same size they had before the birth and never bothered me since. Until now, that is.
A new, tiny one came out after conception. It stung and hurt for a few days. What a nuisance that was! It has stung ever since. Added to that, from the very beginning, the entire anal area has been itchy. Internal piles have also been constant, as proven by regular traces of blood after stools come out. It did not help that despite my best efforts to manage it from diet, water intake and exercise, I was constipated. However, only the bleeding from the internal piles subsided when I had an easy time passing stool. I gave up putting cream on pretty quickly. Although I feel itchy every day, it is not all the time, but rather some moments, usually in the evening. Sometimes I give in, sometimes I manage to breathe it away.
Anxiety
In retrospect, my first pregnancy felt like a breeze. It seems to me we were very relaxed, oblivious and maybe a little unconscious, too. Not to say this was a bad thing. It just made the contrast to how we navigated the second pregnancy all the more starker and evident. Understandably, I believe, given the difficult history of this pregnancy and my age (39), I, we have been more anxious, worrying more.
Anxiety in the first weeks was around the impossibility to get a quick appointment with my gynae, who happened to be away for a few weeks. With my history of ectopic pregnancy, I had been advised to confirm early on the pregnancy was fixed inside the uterus. I had scheduled an appointment with his back-up at seven weeks, so I tried to relax, but could not shake off a feeling of impatience and urgency.
I could not really be happy and hopeful about the pregnancy without this first confirmation. If it was ectopic, there was a good chance I could lose my remaining tube and with it all chance of conceiving naturally. Could we be that unlucky?
A week before the appointment I started feeling mild cramps in the lower abdomen, much like my usual pre-menstrual cramps. I thought it was weird, because I felt them more on the right side, the one without a fallopian tube. No idea if there is or should be any connection. I felt them for a couple of days. Suddenly, they were with me constantly all day long. It felt like (autosuggestion, maybe?) they were radiating in my lower back and down my legs at times. I got worried. Then I started noticing some light brownish traces after peeing, once, twice, three times, every time I went to the toilet, and I became more and more worried.
The following day, six weeks into the pregnancy, I had a first look at my baby. I heard the heartbeat for the first time and confirmed it was in the right place, inside the uterus, on the ER ultrasound machine. All was fine. The urine test came back normal  I got this one ultrasound image that I showed my husband who was waiting for me outside. He had not been allowed to accompany me in the ER because of COVID-19 restrictions. What a relief! And what a surprise to hear the baby’s heartbeat so early on! I had not expected that. It was so alert..
I got this one ultrasound image that I showed my husband who was waiting for me outside. He had not been allowed to accompany me in the ER because of COVID-19 restrictions. What a relief! And what a surprise to hear the baby’s heartbeat so early on! I had not expected that. It was so alert..
The nurses in the ER did not seem impressed, advising me next time to call the ER beforehand. There was nothing particularly worrying in my story. Apparently, if it was not bloody red, there was no reason for concern. The kind, smiling gynae that handled the ultrasound looked equally relaxed about it all.
Once the ultrasound at six weeks and then the medical check-up at seven weeks confirmed all was in order, I started counting down to week 12-13 and the end of the first trimester. I kept reading about signs of miscarriage and all the things that could go wrong. I would not get rid completely of the anxiety around something potentially going wrong thereafter either.
Initially, I told only one friend about the pregnancy, immediately after seeing the positive test. Just to have someone to talk about this in case it all went terribly wrong. Around 8 weeks in, I told my mom and dad. It was my mom’s birthday, so it felt like a good moment to share something like this. We told everyone else around week 14, when we got the pre-natal genetic screening results back.
Nausea
I experienced nausea differently than in my first pregnancy. Still mild; I never actually vomited, nor did it incapacitat me in any way, but a nuisance nonetheless. A nagging sensation that accompanied me between weeks 6 and 12, randomly coming and going at any time of day or night. Plus, I felt hungry all the time; that feeling of having a hole in my stomach that I needed to fill NOW, URGENTLY, or else I could pass through a wall :D.
Frequent peeing
Very much like in the last trimester of my first pregnancy, I felt the urge to pee frequently. It was particularly annoying at night. I was already having trouble falling asleep to start with. I lay with my eyes wiiide open, impossible to close them, until they did. Once I was up and back from the toilet, I was back to square one and it could take me up to two-three hours to fall back asleep. Luckily, my boys let me sleep as much as possible in the morning.
Tiredness
This only further intensified my chronic tiredness and irritation during the day. I felt tired all the time, up until weeks 12-13. Particularly during late afternoon, after picking up my little gosling from the nursery, I felt exhausted and irritable. It was a tough period for my relationship with the little gosling. The occasional naps I took, privilege of teleworking during a pandemic, helped me cope better. They made for calmer, more serene afternoons and our relationship was gentler and less bumpy. Daddy stepped in quite a lot, at play and bathtime and was, as always, a tremendous help. Generally, throughout the pregnancy, he’s been most supportive, encouraging me to exercise – without overdoing it – and to get some rest.
I hardly felt up for any kind of exercise. It felt impossible to keep up the running routine I had started the months before getting pregnant. Whilst I continued going out for my morning walks in the park, more often than not, however, I ended up sitting on a bench, breathless and tired for most of the time I was outside.
Constipation, bloating, reflux
Constipation, bloating and reflux have been an issue throughout. More than in normal times. I tried to eat as healthily as possible, plenty of veggies and fruits. Some days were better than others. Drinking water was always an issue. I made sure I had extra fiber at hand, just in case I needed to supplement my regular diet.
Breast tenderness
Breast tenderness was more problematic this time around. More often than not, breastfeeding little gosling felt uncomfortable, sometimes downright painful. This also rendered our relationship difficult. He found it hard to understand my reluctance and irritation, as I ended up limiting his time at the breast or suddenly interrupting it. It often led to tantrums on one side, irritation on the other.
Nevertheless, I was determined to keep our breastfeeding journey going. I did not want him to feel that he was losing out on account of a new baby coming. Furthermore, I have this strong belief (no idea if it is supported by research or not) that breastfeeding my second one would be easier on my breasts if there is continuity. Maybe avoid some of the early issues with sore, cracked nipples or mastitis or such. We pushed through and adjusted. Only some positions have worked for me. I needed him to face the breast front and center, if we were in an upright position and when lying down, I needed him to be similarly at a 90’ angle, at the same height as my nipple.
Weight gain/pregnancy bump
I gained around 1,5 kg in the first trimester. Sometime around week 12, I woke up one morning and I had a weird looking bump, very high, just under my breasts. It was visible to me when naked, but could easily remain hidden under a loose shirt. At this stage, I still fit into my normal clothes. Breasts seem to grow bigger from early on, but I was anyway still wearing my breastfeeding bras, so no need to adjust on that account either.
I had a medical check-up roughly once per month. Not counting the ER ultrasound, I saw the doctor at 7 weeks and then at 12 weeks. Blood pressure checked; cervix checked to make sure it was tightly shut; ultrasound to check the embryo/foetus. We heard the heartbeat every time. Luckily, despite the COVID-19 restrictions, pregnant ladies could be accompanied, so my husband came along to all the appointments. We had made it to the end of the first trimester. All was in order. We were happy.
My gynae called it a “miracle pregnancy”. Might be because of the little odds he had given me for conceiving naturally with one sub-optimal fallopian tube and a history of ectopic pregnancy, at my age. Might also be because the ultrasound showed that my right ovary (the side missing the fallopian tube) produced the lucky ovule, which was subsequently caught by the left fallopian tube.
The post My (second) Pregnancy Diary: First Trimester Anxiety and Discomforts appeared first on Mommy Goose Chronicles.
]]>The post Spinderella appeared first on Mommy Goose Chronicles.
]]>
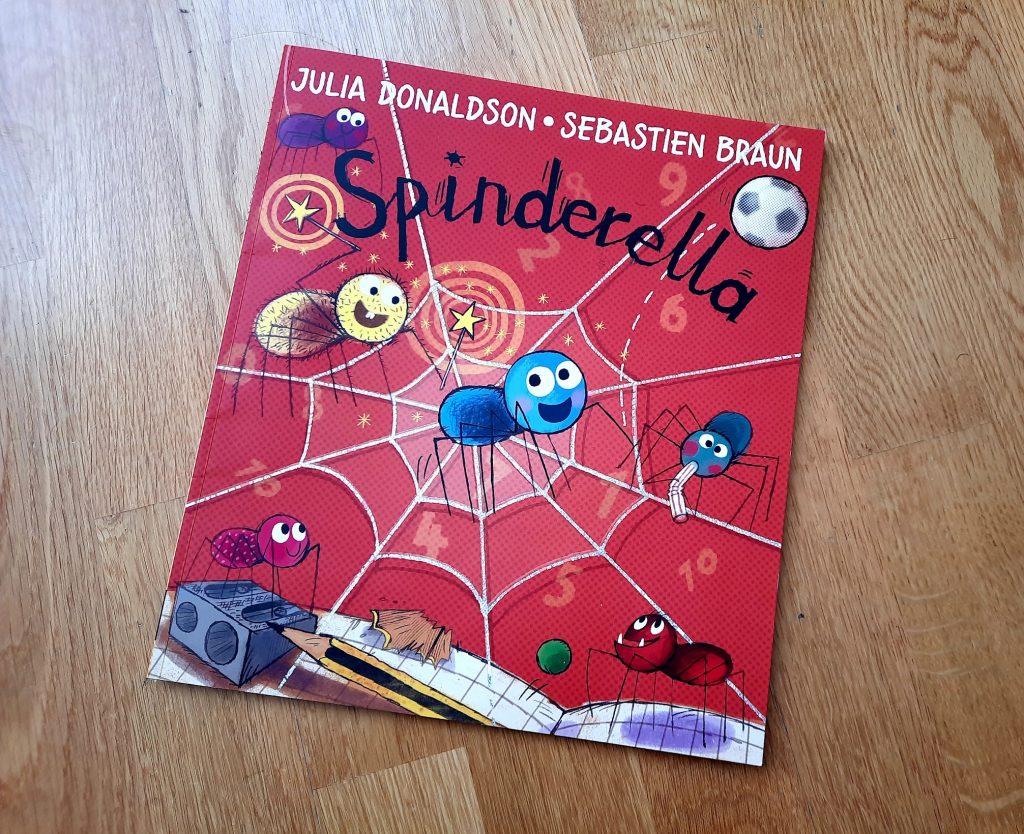
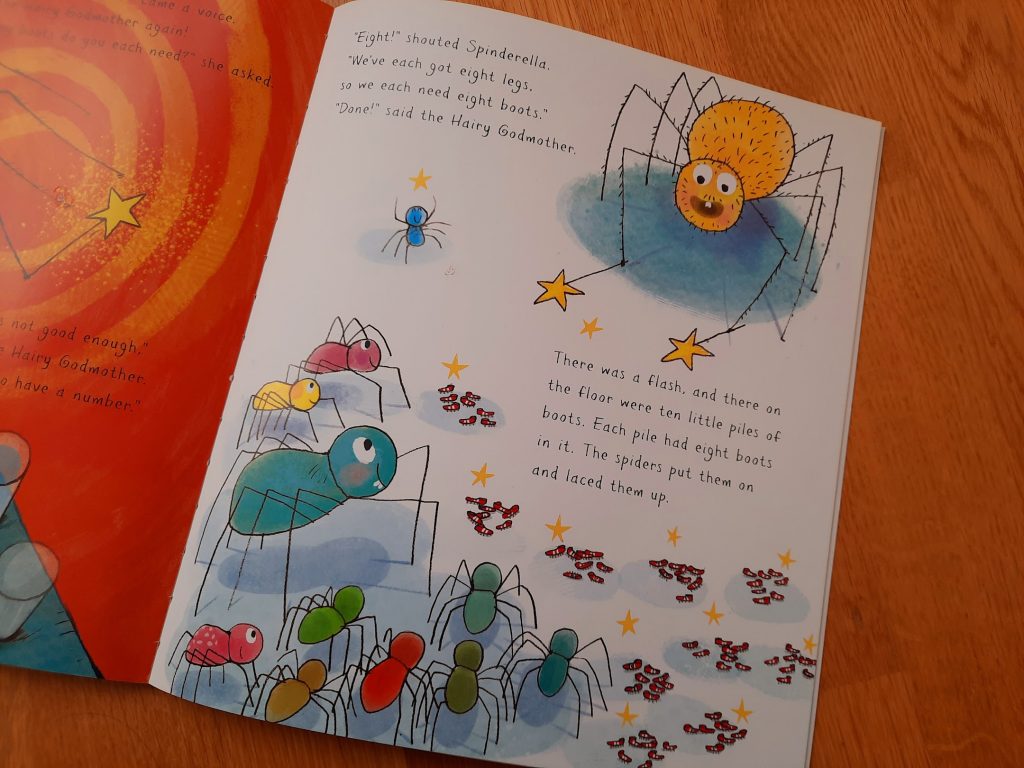
Spinderella is a small, intrepid spider who wants nothing more than to learn about numbers. She finds her family’s absolute disinterest and even disdain on the matter frustrating. Luckily, she lives in a school. With the help of her “hairy godmother”, she learns to count up to twenty, divide up the teams and keep the score at football by paying close attention to the kids at school. She then uses all her newly acquired knowledge to organise her big family into peaceful and fair football playing.
This is the first Julia Donaldson’s non-rhymed story and one of only two collaborations with other illustrators that we read. But such a big LIKE! The first “fairy godmother” encountered – and oh! Such an original one it is :))). A story about the importance of numbers and basic mathematics. How else would one know how many boots are needed to protect the spider’s feet when playing football, for example? A story about fairness and equal chance; encouraging thirst for knowledge and enabling learning; about not getting discouraged and overcoming surrounding ignorance. Bonus: two strong female role models. One determined and in control. The other one brave enough to learn from her mistakes.
Little gosling gets super excited every time the hairy godmother appears. We take turns counting up to 20 together with the kids and shouting “goooooal” when Spinderella scores the winning point. He finds it hilarious when Spinderella’s family counts everything in “lots” and “loads” and shouts “down with numbers!”. I love it when mummy spider respects Spinderella’s knowledge and takes her guidance, as well as the playful positive strong image school and learning this book portrays. We know now what spiders eat and the use of “up/down with” to express like and dislike. I love little gosling’s habit of repeating the new information and explaining it to me and his daddy again and again.. So sweet!
The post Spinderella appeared first on Mommy Goose Chronicles.
]]>The post My (Second) Pregnancy Diary: The Positive Birth Book appeared first on Mommy Goose Chronicles.
]]>I thought “I want to read her books if I ever get pregnant again”… So, once the first 12 weeks of pregnancy were safely behind us), I diligently ordered a copy of her first book, “The positive birth book”.
This is an informative and empowering reading, particularly for first-time moms-to-be or mummies who are looking for ways to have more control over and improve on their subsequent birthing experiences. With exposure to the medical systems in three different countries on two continents, with different approaches and options offered to women to give birth, I found the book an especially useful read for women who give birth in traditionally highly medicalised or interventionist settings.
It can help ease a lot of the anxiety and fears first time moms-to-be experience. It challenges some of the common misconceptions and negative perceptions around birth. It is packed with research-based data, medical and birthing experts’ opinions and all kinds of personal birthing stories. Although rooted in the anglo-saxon ways of doing things, there are many important lessons that can be drawn to improve on birthing experiences of women everywhere.
I have a positive recollection about the birth of my son: a quick, natural birth, in an informal, quiet, cosy, non-medicalised setting, with a midwife who only made her presence known when absolutely necessary, my husband next to me. The book reinforced my belief that I had done the right things the first time around to help me birth my baby as I wanted and the wish that my second birthing experience resembles the first one. I noted down a few tricks for labour and preparation for labour looking at how I could improve on my first experience.
I definitely want to practice more and regularly (and starting much earlier) staying into the relaxed zone. I remember how difficult it was to stay relaxed and focused on breathing during the active phase of labour. I felt out of control of what was happening. I thought about making up my own affirmations and practicing one or two visualisations of my own (e.g talking to my baby, imagining moments together with baby and little gosling, cuddling, singing or reading together or just spending time outdoors). I would also like to try and be more present during labour, including active labout, taking mental notes of my sensations, for an accurate picture of my birthing story.
I will make sure to have the image of different birthing positions at hand and put a note to move more. During my first labour, I was quite static. This worked amazingly well for me during the first stages, being all relaxed, either sleeping or in the bathtub, listening to my relaxation tracks. The later stages were messy and although I tried a few different things, maybe, just maybe, moving around more (maybe dancing? :)))) and trying a richer variety of positions could render it more manageable.
More importantly, the book inspired me with two intentions (may be common sense to many, but not obvious to me):
- Be more assertive in my interactions with doctors/caregivers. Ask questions; discuss options and alternatives; ask for pros and cons. Not be afraid to say “no” or “I want to do things differently”, “I want to wait a while longer” if something does not feel right. One thing I would definitely be more inquisitive and assertive about is the idea of a possible induction or a membranes sweep. Little gosling was born at 41 weeks exactly, a few hours before a planned membranes sweep which we had accepted without much questioning, but very anxiously, purely trusting our midwife.
- Stay open-minded and flexible about the way in which birthing could go. If my plan A cannot happen (a natural, full-term, non-medicalised birth), there are ways to make other courses of action more palatable. I intend to prepare myself as much as possible, so as to have a birthing experience that I can feel good about and remember without angst.
The post My (Second) Pregnancy Diary: The Positive Birth Book appeared first on Mommy Goose Chronicles.
]]>The post Aventurile ramei Oli appeared first on Mommy Goose Chronicles.
]]> has spent more time with a runny nose than with a clean, dry one. As such, we’ve had many conversations about mucus, germs and the importance of eating fruits and veggies for a strong, healthy, mucus-free organism. “Aventurile ramei Oli” (The adventures of Oli the worm in its Romanian original) have been of great help to visualise things in a playful manner.
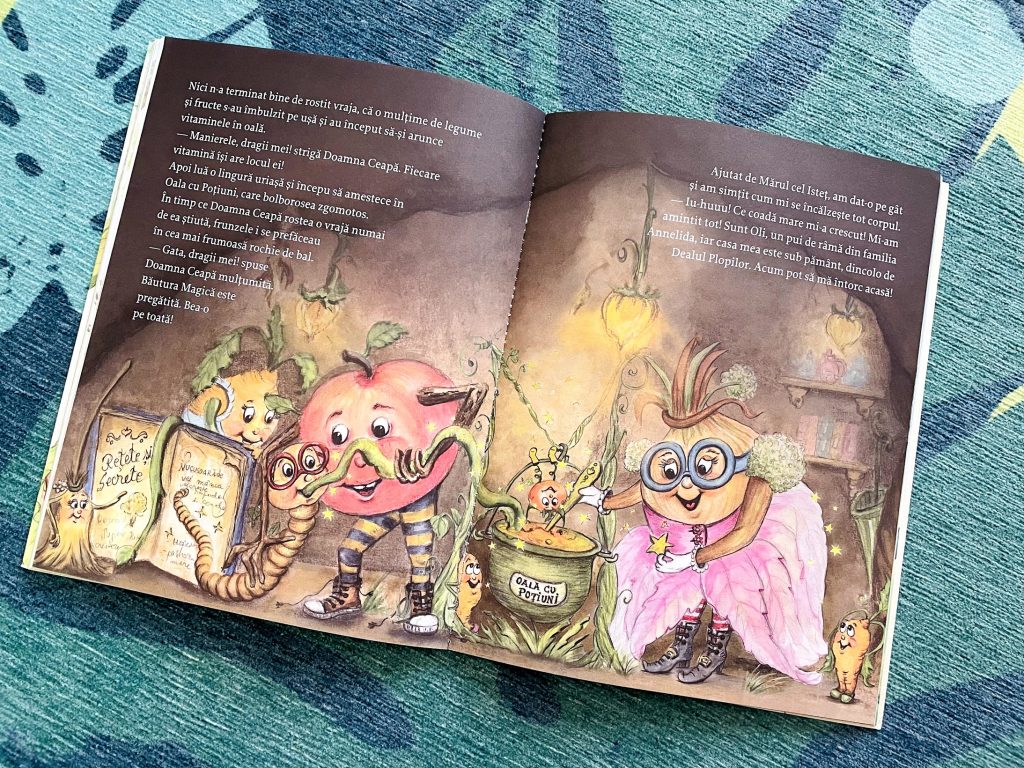
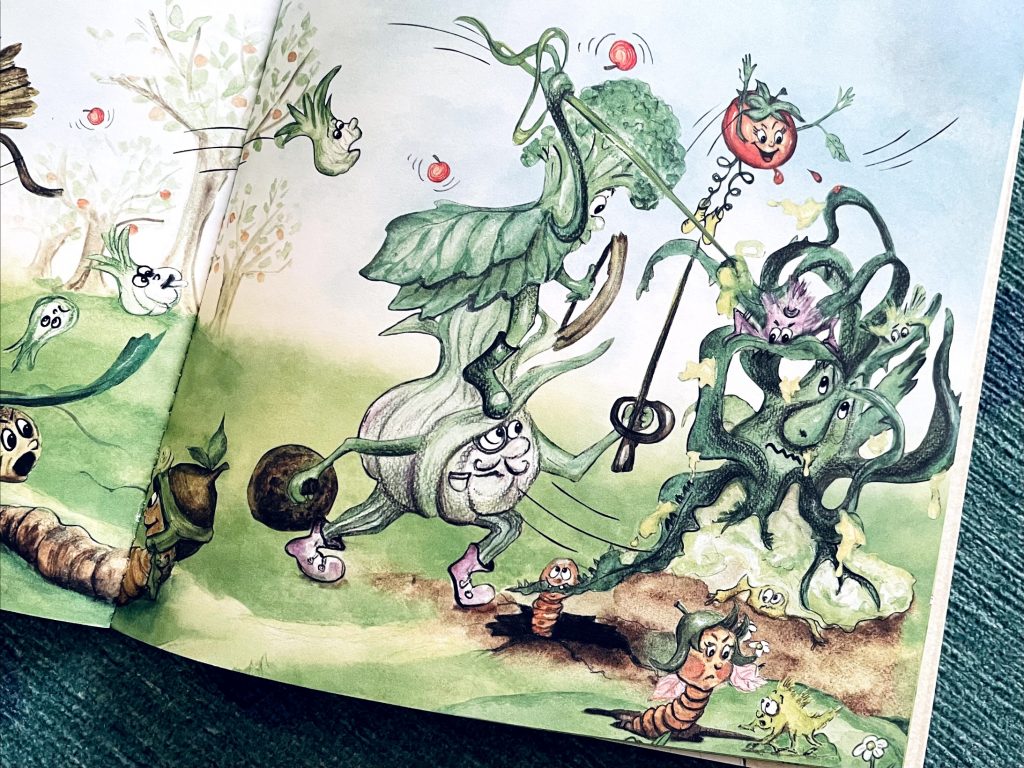
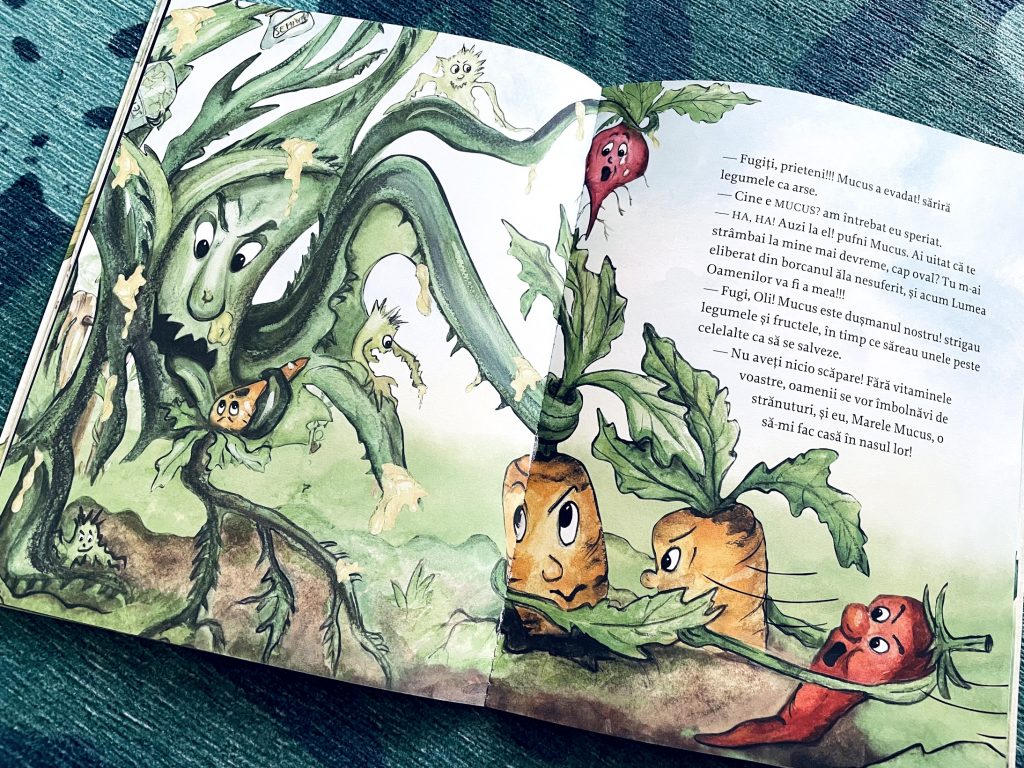
has spent more time with a runny nose than with a clean, dry one. As such, we’ve had many conversations about mucus, germs and the importance of eating fruits and veggies for a strong, healthy, mucus-free organism. “Aventurile ramei Oli” (The adventures of Oli the worm in its Romanian original) have been of great help to visualise things in a playful manner. Oli is the cutest worm, with those big, red glasses and contagious smile, who unknowingly lands in the Magical Garden, falling from an unfriendly beak. He makes friends with a Witty Apple who takes him to Madam Onion, the knowledgeable garden healer, master of the vitamins’ secrets and slayer of germs and viruses, to have his broken tail mended. Accidentally, he knocks down the jar where Mucus is locked away from the world. A fierce battle ensues between the inhabitants of the Magical Garden on one side and Mucus on the other.
Great opportunity to learn how useful and beneficial earthworms are to our gardens, true super-heroes, much like the broccoli, onion and garlic that put their strengths together to annihilate Mucus. Even more so as little gosling is not a fan of tomatoes, onions or garlic. Tomatoes, it beats me why, because he loves tomato sauce and ketchup. The other two he finds too spicy (“maybe I’ll like them when I grow up”), although he does occasionally taste some onion heart, but only because he can dip it in the salt and he loves that ;).
It’s an amazingly fun and playfully informative read. The scattered little poems and witty names are charming. The characters each have their own distinct personalities and add flavour to the story. The panicky Lisp Tomato and Madam Onion’s Whisk are my favourites. The illustrations marry well with the text, perfectly depicting the conviviality of the garden community.
The post Aventurile ramei Oli appeared first on Mommy Goose Chronicles.
]]>The post My laparoscopy experience appeared first on Mommy Goose Chronicles.
]]>One of my tubes was completely compromised, the second one partially compromised and the uterus half covered by adhesions. I was told this was likely a consequence of the (many and invasive) post-birth interventions I had undergone.
The procedure was scheduled for 9 a.m. on the Friday before Christmas 2020. I was invited for the pre-op consultation days before, with a nurse and an anesthetist. More blood tests and an EKG. I was told to shower the night before and again the morning of the intervention, washing thoroughly my body, gradually advancing top to bottom, with iso-betadine received. I was to avoid any fragrance, perfume, cream, as well as shaving the few days prior.
I went in at 7 a.m. Little gosling was still sleeping. My husband kissed me goodbye and I took the metro to the hospital. It was still very dark outside and the air was crisp. It felt kind of lonely, but we had no one to ask to babysit. Mr Obama was reading to me from his book in my headphones. I carried a backpack with me (completely pointless, as it would turn out, but I was following the hospital’s recommendations) – phone, charger, Ipad, headphones, a book, a pj, slippers, a towel and a change of underpants. I was, apparently, geared up for boredom :))) during my scheduled one night stay in hospital.
We had explained to little gosling (2yrs 8 months at the time) that mummy would be away, in hospital, undergoing an intervention whilst asleep for a day and a half. It was the first night we spent apart since his birth. No visits were allowed (COVID safety regulations), but we could talk over the phone. Daddy would be taking him to and fro the nursery, read to him the next book from our book Advent calendar and he could sleep the entire night in mummy and daddy’s bed. He seemed to understand, although he did ask for mummy and for tzatzi a couple of times during the evening/night.
After a quick registration procedure, I got a white plastic wristband, complete with a barcode (which was scanned every time I was moved and changed rooms) and my photo on it. I proceeded on my own to the extremely quiet maternity ward. I checked into my private room (the only way to guarantee that the intervention would be assigned to my obstetrician of choice) and changed into the hospital gown and panties I was given. A training nurse came in to shave my lower abdomen (at pre-op I was advised to avoid any shaving/hair removal the preceding days) and helped me put on compression socks. I drank the Xanax she left for me with just a small sip of water. I was feeling thirsty and hungry by now. I lied down. I read a bit, but mostly dozed off, waiting to be taken to theatre. I felt quite emotional, with tears coming to my eyes. I put on the new mask given by the hospital, just in case. I watched the short video my husband had sent with my son, delaying getting dressed for school, singing and saying hello to me into the camera. So sweet!
The scheduled time passed without anything happening. At 9.45, a stretch-bearer took me down, scanned my wristband and “parked” me in the big waiting room of the operatory block. It was a big hall, with mobile beds parked perpendicularly to the wall, separated by curtains. Nurses, doctors and “bed couriers” were coming in and out. More patients came and went almost immediately, their beds pushed by their operating nurses or anesthetists. I stayed put. I kept quiet and still, listening to the chatter next to the other beds. I was drowsy and had no sense of the passage of time. I asked the nurse in charge of the waiting room for the time – 11.15h. Hmmm… No idea when all that time had slipped by. It took a while longer before the anesthetist came, apologised for bringing me down too early and pushed me towards the theater. I climbed onto a higher mobile bed, my wristband was scanned again and off we went.
In the very well lit theater, the table stopped under a huge light. A nurse put electrodes to monitor the heart rate on my chest and somewhere on the back, the blood pressure thingy, then wrapped my right arm safely alongside my body. The anesthetist installed the drip, whilst telling me a joke from one of Louis de Funes’ movies. I was covered with an extra green blanket – I was cold and shivering. My hand started to hurt when the drip started flowing. The doctor slowed down the flow. He held a mask on my face; my hand started to hurt all the way to my elbow and I lost consciousness before I could finish telling him that.
Next thing I know is waking up with pain in the lower abdomen, much like strong menstrual cramps. I was feeling heavy. Had this constant need to clear my throat to be able to speak. I was feeling groggy. A nurse was busily moving around my bed, hanging things. I could feel pressuring and letting go of my arm, followed by a beeep, the thingy measuring my blood pressure. I was in a haze for most of the time I was conscious in the recovery room. The nurse kept talking to me. She gave me painkillers and placed a hot water bag on my tummy to ease the pain. At some point, I located a clock on the wall in front of me – 14.15h. I tried to calculate how long I had been under, but found it impossible to be precise. At 11.15 I was still in the waiting room, but my sense of time had already been altered by then. And who knew how long it had taken me to open my eyes after the procedure?
I thought to check the bandages, to make sure things hadn’t gotten wrong and there was no big cut. I slowly took my hand under the blanket and felt small pieces of bandage here and there on my abdomen. Oh, good! I felt relieved. It had stayed laparoscopic…
I could feel the hotness of the water bag and kept moving it around my tummy. At one point, my bed was moved to one side, waiting for a stretch-bearer to take me to my room. A different person, chattier, took me back up. He made small talk, but I can’t remember what it was about. It felt like my stay in the recovery room had been very short, but by the time I was back in my room it was past 16.00h. I sent a quick message to my husband.
My throat cleared out quickly. I still felt the menstrual-like cramps and some stingy sensations alternating between the cuts, one at a time. I pulled up my shirt and counted 5 small squared bandages: 1 in the navel, 3 in the lower abdomen (middle, left and right a bit higher), one above the navel on the left side. I was intrigued: why so many? Why the one above the navel? I suddenly felt hot and I took away the additional blanket they had put on me in the theatre.
A nagging sensation to pee came to me. A nurse helped me get up slowly from the bed and then waited outside the bathroom door. I pulled up the hospital shirt and looking down, there was suddenly more blood than I had anticipated and it started flowing down my legs, staining the compression socks.. I asked for help, I was too slow… I sat down, but did not manage to pee in the end. The nurse called for help and they helped me back to bed. I felt dizzy and a bit nauseated. “Call us when you want to get up again”, they told me.
The nurse came in regularly to check my temperature, blood pressure, the bandages for any further bleeding, as well as for any vaginal bleeding. All normal. She warmed up my water bag as well. That helped a lot.
I called my husband and parents. They had been worried. I had gone into surgery three hours later than scheduled, so my husband had immediately feared complications. He had called the ward to ask after me. I could sense my parents were also relieved. I wrote back to my best friends who had left messages of encouragement during the day.
At some point, the pain came back. The perfusion got stuck and the nurse could not manage to fix it. She called the anaesthetist to ask whether she could change the whole thing, but couldn’t reach him. He had just passed by my ward minutes earlier and was possibly on his way home. The surgeon told her she could it take off completely and give me pills instead. Dafalgan forte every three hours or so. I also got a pill, good tasting, to put under my tongue and suck it. And, at some point in the evening, the much dreaded anti-clout injection in the belly came upon me.
The surgeon stopped by to see me in the evening. He gave me a quick summary. He had taken out the right tube. He had saved the left tube, but “it wasn’t exactly beautiful”. He had cleared the adhesions in the uterus and he had spread a gel all over to prevent further adhesions from forming. Half of the uterus was closed; “all sorts of things had happened inside” he said. He told me to drink a lot, stay hyperhydrated. Gave me the medical leave paper and prescribed me antibiotics for the next five days.
Afterwards, I dozed off, woken up only by the nurse’s visits. The night nurse told me to drink water and call for help to go to the toilet. I had to pee before midnight. I drank 1l and a half of water and waited… two hours until I felt any need to pee, not remotely as pressing as I would have thought after drinking that amount of water in one hour! Victory!!!
Around the same time, my shoulder started to hurt, around the clavicula. Sharp. Numbing. It came and went. It felt particularly poignant when I stood up and went to the toilet. No more dizziness, but it came with nausea. Keeping it warmly tucked under the blanket helped. I rubbed it with my other arm and put my head on it, kind of like hugging it. Pain in the abdomen was now localized between the five cuts, not anymore focused on the lower abdomen. It was surprising to me to learn this was absolutely common after a laparoscopy, an effect of the CO2 they put inside the abdomen to dilate it during the intervention. It takes a while to make its way out of the system.
I went to sleep listening to Mr Obama. Between midnight and 6.00 all was quiet. I woke up a couple of times, either to go pee or to adjust my position. My feet hurt, swollen in the compression socks.
Early morning, after the usual checks (everything was in order, very little vaginal bleeding, bandages same as the previous day, no fever and my usual low blood pressure), I peed again. It seemed like “the” milestone to meet, my nurse was very interested in it. My bandages were changed. I decided it was time to go for an extended walk around the ward. I felt bloated. My shoulder pain kept coming and going, particularly when I stood up. It went all the way from the stomach, with some nausea, through the diaphragm, all the way up into the right clavicula and then through my right arm all the way down to the pinky finger. I had read that walking should help.
The anesthetist came again and prescribed me a diclofenac for my shoulder pain. A kinesitherapist subsequently came by to check on my shoulder. All was within parameters.
I left the hospital on my feet right after lunch. My husband and little gosling were waiting for me outside. The little one had fallen asleep in the car seat. My backpack felt heavy. I realised I could have gone with just my phone and headset to the hospital. Anyway, better to be prepared for the worst.
The laparoscopy was a success. The best result possible had been achieved, no miracles. Out of the hospital, I felt no more pain in my abdomen. However, the pain in my right shoulder was strong and numbing. The worst was between 18 – 36h post-op. During the same period, gases were also quite painful, particularly so when lying down. The second night after the intervention was difficult. Without the adjustable hospital bed, my improvised pillowed backrest was much less comfortable. It was also a struggle to keep little gosling at distance from my tummy. It took a lot of explaining as to why we needed to be more careful for a while.
Later on, together in the bathtub, with the bandages off and the cuts still visible, little gosling would ask what happened. I told and retold him how those many tiny cuts on my tummy had come about on the occasion of our first and only night apart, so far.
Four days and a half after the laparoscopy, we flew home for Christmas. A two hours and a half flight. I was anxious, as I had read that gases in the intestines dilated at least 30% at great heights, and was afraid of pain and discomfort. The surgeon had reluctantly given me a green light to fly; he would have preferred I waited, but it was already the 23rd of December. The International Civil Aviation Authority indicated on its website it was safe to fly 2 days after a laparoscopy. So, we took a chance. All went well, no sensations whatsoever. I spent two weeks convalescing at my parents’ home, reading books and doing little of anything else, whilst little gosling was enjoying his grandparents and their garden and animals, in the mild winter weather.
The post My laparoscopy experience appeared first on Mommy Goose Chronicles.
]]>The post My Unexpectedly Bumpy Road to a (Viable) Second Pregnancy appeared first on Mommy Goose Chronicles.
]]>My period properly returned one year after little gosling’s birth. I had felt some cramping from six months post-birth and some light occasional spotting from 9 months post-birth onwards, but it was around 12-13 months that it came back in all strength.
At around 9-10 months post-birth I had seen a GP. He advised a general ultrasound to check that all inside of me was ok. I had an ultrasound of the abdominal cavity, including ovaries and uterus, and everything was deemed in order. As I had expected, he suggested extended breastfeeding could delay another pregnancy. I had no intention of altering our breastfeeding journey, so I plainly ignored that part.
I had (and still have) a very positive recollection of my birth experience (shared here), but the negative emotions, the anger and anxiety that surrounded the post-birth complications and the way in which they were medically dealt with (my story here), took a while to fade away. I still remember conversations with my husband the weeks and months after it was all over.. He was seriously considering avoiding a second pregnancy and opening to the idea of adopting instead, just to avoid the risk of reliving the first post-birth experience. The idea of giving birth again brought me to tears.
I did not see a gynae for a while after the birth experience. The doctor who had followed my pregnancy had not answered my messages after the birth of my little gosling and that had made me feel disappointed and distrustful. I kept recommending her to other women around me, but I did not feel comfortable seeing her again. Neither me, nor particularly my husband felt comfortable going back to the gynae who had managed by post-birth complications. We blamed her for having to go through a second curettage and an abdominal surgery. The expat women around me saw one of these two doctors and I felt uneasy about seeking advice from strangers. I kept postponing seeing a gynae and felt reassured with my GP’s advice.
With all these in mind, we felt ready to try again. We were quite laid back about it, much like the first time, when we had just stopped using any contraception and let it happen (which it had fairly quickly, with no stress, just a few months later). This time we kept a closer look at the calendar. I was expecting it to happen as easily and naturally as it had then. It did not.
I remember seeing my GP at around 13-14 months post-birth. He made me pee on a stick, can’t remember why. What I do remember, however, is the deep sense of hope, followed by a huge disappointment when it came back negative. He suggested again that breastfeeding would be an obstacle to a second pregnancy and advised me to start tracking my ovulation to actively help my chances. We did that for a couple of months. I was ovulating each month, but no pregnancy ensued.
I got curious and stumbled online upon the concept of secondary infertility. This is the inability to conceive a child (or carry a pregnancy to full term) after previously giving birth, assuming the previous birth occurred without fertility treatments. Secondary infertility typically is diagnosed after trying unsuccessfully to conceive for six months to a year. No idea whether this timeline holds for parents of all ages (we were both 35+). None of the medical professionals I saw in the past year used that term concerning my situation, but I could not have been very far. It appears to be a phenomenon as common as primary infertility. It was a surprising discovery for me. The fact that it was a medical condition labeled as such somehow reassured me. It was something that happened. I also just had a colleague giving birth to her second child completely unexpectedly in her early 40’s, more than ten years after the first child and without purposefully trying to have a second child. So, we continued trying, more or less organised about tracking the ovulation periods.
A few months later we moved back to Brussels. Little gosling was 18 months old. I had the intention to see my regular gynae, but kept postponing for until after little gosling was settled into the nursery; after we came back from my grandpa’s funeral; after the one month Christmas holiday with my parents in Romania; after we had settled into our newly rented apartment…. Then the pandemics came upon us and somehow, going to the clinic and seeing a doctor for non-urgent matters became close to impossible for the first months. Ten months passed before I actually got to see my gynae. Little gosling was 2 years and a half by now.
The check-up was routine-like to me. I shared my story with the gynae – the expression of cautious disbelief on his face upon hearing how it all had happened! I asked whether there were any obstacles preventing me from getting pregnant again, as we had been trying for many months with no result. I remember asking this more out of curiosity and to check a box (since I was there anyway…), than out of serious concern that something could be wrong. We kept trying, without any pressure on us; we wanted a second child and gave ourselves time until we turned 40, but put no pressure on ourselves.
The gynae very calmly explained the ultrasound revealed something on one of my tubes that needed to be further checked. He had also noticed adhesions in the uterus, a rather common occurrence following surgical interventions like those I had experienced, he explained. He recommended both a hysteroscopy and a hysterosalpingography, which he described as specialised medical imagery tests, one resembling an ultrasound with a telescope going inside the uterus and tubes, the other a localised X-ray of uterus and fallopian tubes with a contrast substance. He also prescribed some blood tests. His tone and demeanour were calm and not a bit alarming. He said we would figure it out. As always, he would only call me if there was a problem with the results. I left the office without any alarm bells ringing.
I gave blood the same day. The following evening the gynae called me. The blood tests had detected the presence of the pregnancy hormone, but in a quantity that signalled an unhealthy pregnancy. I was shocked and froze on the spot (I had come out of the supermarket to take the call), trying to process it all. I had just had a normal period two weeks before. Gynae said it must have been a false period; the pregnancy was several weeks. And the embryo must have been what he had detected in my tube during the ultrasound. He called me back the next morning to redo the blood tests. If the hormone levels were going up, an intervention could become necessary in order to remove the ectopic pregnancy. If hormone levels were going down, there was a chance I could get away without an intervention.
I shared the news with my husband. He was equally taken aback. We had not seen this coming. We were dismayed. All I knew about ectopic pregnancies was the experience of a colleague who had undergone interventions to remove both her tubes following two consecutive ectopic pregnancies and had been left unable to conceive naturally. I found the prospect of another curettage daunting. It brought back all the anger and frustration from the post-birth times. It was all I could think about. I felt guilty and blamed myself for waiting so long before seeing a gynae. If only I had seen my gynae upon returning to Brussels! I blamed the gynae who had dealt with my post-birth complications for not alerting us to the risk of uterine adhesions and insisting on regular, frequent follow-ups. She must have known uterine adhesions were a common occurrence and a strong possibility in my case and that they could lead to possible difficulties for a second pregnancy, if left unchecked. Why didn’t she take the trouble of even mentioning this to us? If only she had…
I shared the news with a couple of my mummy friends for support and alerted my mom – in case of an intervention, we planned on flying her over to help with little gosling. One thing we had learned from prior experience is that one knows how you go into the theatre, but there is no guarantee on how one comes out and how long the recovery takes.
The next morning gynae did another ultrasound, to check whether there was any change with the tube. Everything looked the same it had days before. He explained the risks carried by an ectopic pregnancy as advanced as mine – more than six weeks. Rupture of the tube, internal bleeding.. And there’s a limited timespan before it ruptures the tube. An intervention, if required, would need to take place within days, to avoid the risk of the pregnancy rupturing the tube and provoking further damage.
I redid the blood tests. That same evening the doctor called with “good” news. The hormone levels had gone down (from 20 to 1), meaning the pregnancy was dying on its own. No intervention was needed. I felt relieved. And I still had my tube. The embryo would be expelled by the body at the next menstruation that would take place in 10-14 days. He insisted for me to make the appointment for the two medical imagery tests immediately after that. And I did.
A couple of days before the date for the tests, I started developing COVID symptoms. That week, little gosling’s nursery had been quarantined for a week upon detection of the virus among the carers. It was a Sunday. The on-call doctors told me to continue monitoring symptoms and see a GP if they persisted/got worse. The night before my tests, I developed a light fever. I called the hospital the next morning and was advised to cancel my tests and call back the following month. Both tests need to be performed within a certain interval at the end of the period, so one can’t really plan much in advance. Add to the uncertainty I felt about a COVID infection the frustration of having to delay the tests and wait another month. Luckily for us, we sailed rather easily through COVID, with only mild, albeit disconcerting symptoms.
35 days passed without any period. No, I was not pregnant. I was worried. What did it all mean? I went to see my gynae again. He confirmed the situation was unchanged, as well as the absence of a pregnancy. He revealed a bit more on the occasion, saying the tube where the ectopic pregnancy had been was dilated and I really needed to do those imagery tests to have a better look at them and decide the course of action. Particularly so if I wanted another baby. But even without it, it would need monitoring. There was the possibility of a rupture of the tube, in which case I risked an internal haemorrhage. According to him, the period delay could have been due to COVID and prescribed me some pills (Lutenyl) to bring about the menstruation. One pill and one day later, there it was.
It was a difficult period for both myself and my husband. We were feeling discouraged. Angry that all this should have happened to us. My husband was quite affected by the ectopic pregnancy and the idea of pregnancy loss. A chance lost. At the time, I was so shocked and so anxious about the possibility of yet another curettage and losing one tube, that I didn’t even fully realise there was a pregnancy in the middle. My knowledge of being pregnant was too-short lived and overtaken by other kinds of fears and thoughts, that it hadn’t really sunk in. We felt disheartened, lost. Anxious that we were losing so much time to get those tests done and have it fixed. We started thinking of all the other times my period had taken longer than the post-birth average of 28 days, wondering whether some of those had been ectopic pregnancies that just died on their own. After all, if I had gone to see my gynae a few days later, we would have never known about the ectopic pregnancy.
I had the tests done less than a week later. Another gynae. More shocked looks upon hearing the story of my post-birth complications. Another vaginal ultrasound prior to the tests, to make sure there was no pregnancy anywhere and to have an idea about the baseline. He said something to me that felt reassuring: I still had plenty of ovules left. At least that..
I had the hysteroscopy first, in the morning, on the last (6th) day of my period. I had taken some painkillers, as instructed, one hour or so before the intervention. The setup was very much like during a regular consultation, although it was in a special room. I was on my back, legs in the stirrups. Something was placed inside to keep the vagina open whilst the gynae worked his way up to the uterus with the hysteroscope (a tube with a telescope at its end), while watching everything on the screen. It wasn’t pleasant, but it did not hurt. I kept looking at the screen. All I could see was a pinkish tunnel. The gynae was having trouble advancing and said something about the cervix having an unexpected bend. Can’t remember much of the sensations really, apart from a general and gradually stronger discomfort with the tube moving inside me. Finding a way to make the tube advance took a while, maybe one or two minutes, maybe more. It felt very long to me, especially as I was feeling myself fainting. My blood pressure, quite low usually, got lower and both gynae and nurse started fretting a bit, the nurse rubbing my face and hands with something cold, holding my hands and talking soothingly, the gynae trying to speed up the procedure. I was almost out of it, when the doctor said he was wrapping up. He could not see much. Hopefully, the hysterosalpingography scheduled for a few hours later would feel better. In any case, he said, that would go much faster. He insisted not to forget to take my painkillers beforehand. I felt weak, but colour was coming back into my cheeks and a few minutes later I made my way back to the restroom to get dressed. Out of reflex, I locked the door after me, with both doctor and nurse instantly crying I should unlock it. What if I fainted in the bathroom and I needed help?!
I went back home, weary about the second procedure. Bought the exact painkillers the doctor mentioned and went back in the afternoon. It was during the second COVID-19 lockdown, so patients could not be accompanied to hospital appointments. The hysterosalpingography was done in one of the X-ray rooms and I laid down on my back on one of those big tables, with my feet up. It was super quick, it was done in no time. The contrast substance did not have much space to spread. Same doctor as in the morning told me one tube was completely blocked; the other one was also partially blocked and the uterus was full of adhesions. He spoke in a way that let on that the most likely course of action for a second pregnancy would be a laparoscopy, possibly followed by IVF. But my regular gynae would get the images and his report and would talk me through the options.
I left the hospital in tears. I felt anxious and hopeless, fearing the laparoscopy and losing my tubes. I could not make out what it all meant for the uterus. I called my gynae a few days later and he confirmed we needed to schedule a laparoscopy to see what could be done about the tubes and uterus. However, due to COVID constraints, he could not be definitive about the date. He was super prudent, not venturing into any speculations about the outcome. He’d only know once he got inside. It did not feel reassuring at all. We were in a state of constant anxiety about it. And impatience. It felt like it was dragging on and on..
I started reading about IVF procedures, thinking it would help ease my weariness. In hindsight, it was premature and only added to my anxiety. It sounded intrusive (needles would be used), uncomfortable, if not outright painful, the result was by no means guaranteed. It did not sound like something I was prepared to do.
The laparoscopy was scheduled for a few weeks later. A couple of days before it was moved back a week – the Friday before Christmas. I asked the gynae to give me a call and walk me through the intervention. I was very weary. I wanted to know more about what he expected to be able to do. One of the tubes was dilated a lot and full of fluid, a condition called hydrosalpinx. It was over 6.5 mm in diameter (compared to its original 1 mm) and the chances of saving it were aleatory, according to medical literature. The second tube was also in a bad state, a few mm dilated, but in a better shape than the other one. He would do his best to save them. The uterus was half closed, covered in adhesions. He would clear them and put on a coat of gel to protect it against further adhesions.
I recounted my laparoscopy experience here. The outcome was probably the best one could reasonably expect. One tube was lost, the second one was saved. He had also managed to recondition the uterus.
I went back to see my gynae a month later. He walked me through the procedure, showing me photos. I don’t recall much of what I saw, only the distinct sensation that it wasn’t pretty. The next thing he said startled me. He asked whether to send me already to start the IVF procedure. I was not ready to go down this road and my husband was fully supportive. I felt discouraged that conceiving naturally appeared less of a chance than IVF, or so I deduced from the doctor’s advice. I asked him whether it was really necessary at that stage. He said I was in a better condition to fall pregnant than back in August/September, before the ectopic pregnancy. Advised to give it a try for 3-4 menstrual cycles and prescribed pills to help with ovulation. He was also very clear that given my history, it was wise and important to detect the pregnancy early, to make sure it was fixed inside the uterus.
At this point, I was really discouraged. I saw no reason to hope and thought it unlikely that we would be able to conceive naturally. We decided to try for a few months and then see again whether my feelings about IVF changed. We talked about IVF and decided we were both ok with not going down that road, if I still felt uneasy about it.
It was end January. I had already had my period that month and lost the window for the pills this time. I tracked my ovulation, but none was detected. I took the pills in February and again in March. Afterwards I stopped. The pills coincided with the surge of painful pimples all around the vaginal area, vulva and area, which lasted quite a long time and were uncomfortable day to day and particularly dissuasive for any sexual activity. In my mind I established a quick causal link between the two – it was hormone-based and the only other time in my life when I had experienced something similar had been in the weeks immediately following the birth, when hormones are supposedly still running crazily wild. Ovulation happened those two months, but I suspect I had started tracking it too late, albeit following the tests’ instructions.
After my April period, I started tracking my ovulation earlier. After two empty tests, the third one showed the start of the period with optimal chances to conceive (a few days in advance to the calendar). Three days of ovulation in which we applied ourselves to the job :). On the day that should have been the second one of my following period, I did a pregnancy test. It was positive.
Both my husband and I were cautiously happy. We did not want to get our hopes up before confirming that it was a viable pregnancy. Our thinking was: first make sure it was fixed in the right place; then make it through the first trimester; then wait for the pre-natal genetic screening to come back ok. Only then would we take a breath and allow ourselves to truly enjoy it.
What followed were two weeks of feeling pregnant in a completely different way than the first time. Small, but constant discomfort was the norm. Tiredness. Anxiety. Imagining all the different ways in which things could go wrong. Finally, a healthy baby girl is growing inside my tummy, with a family of three waiting to meet her when she is strong enough and ready to come out.
The post My Unexpectedly Bumpy Road to a (Viable) Second Pregnancy appeared first on Mommy Goose Chronicles.
]]>The post Jabari Jumps appeared first on Mommy Goose Chronicles.
]]>The story captures in all its details the emotions Jabari goes through in attempting his first jump from the diving board. His initial courage (“how hard can it be?!”), his doubts, his fear and anxiety, finding excuses to delay the jump, whilst trying to put on a brave face, the courage he draws from his dad’s empathetic attitude and finally, the excitement of the accomplishment. Love dad’s attitude – encouraging in the key moments, without being intrusive or insistent. So effective! What a great bond the two of them must share! Great for modelling parental behaviour when little ones deal with challenges.
After reading this, little gosling has become fond of squeezing. He gets it could be a part of a secret language we can develop together. And he’s been asking whether we could find a pool where young kids like him can swim and do exercises in water (alongside mummy and/or daddy, certainly). So, there’s some homework for me 
The post Jabari Jumps appeared first on Mommy Goose Chronicles.
]]>The post Sully the Seahorse appeared first on Mommy Goose Chronicles.
]]>
Sully feels anxious and intimidated to compete against his colleagues in the sea school contest. He’s not particularly good in any of the disciplines in the competition (that is being polite). He tries to avoid participating, but Miss Trout encourages everyone to just try their best and he feels obliged to do so, all the while fearing and knowing he’ll come last. He wishes he could have one of the talents his colleagues possess.. Until he amazes everyone with his ability to change colour and become invisible in the sea, in face of danger from being caught by a diver. He realizes, then, how special he is :).
This is a cute, lovely rhymed story, populated with sea creatures, full of emotion, with brightly coloured illustrations. Sully is relatable and one can’t help wanting to hug and comfort him. For some reason, little gosling is hooked on Miss Trout, the teacher. He gets excited at every start of a race “On your marks, ready, get set… go!!!” and he’s fascinated by the shadow of the boat underwater. He calls it “the book with the shadow” On one of our readings, I told him the words in the book : “you are amazing” and he said “no, I am not amazing, I am a baby!” :)))
Little gosling has his own little pink seahorse buddy, which he carefully chose himself after our visit summer 2020 to Sea Life Blankenberge, where we saw some less glamorously coloured seahorses.
The post Sully the Seahorse appeared first on Mommy Goose Chronicles.
]]>